Obamacare “Observations”
Team Obama brags that that the readmission rate of patients to hospitals has been dropping. It has. And that was one of the goals of Obamacare.
Are congratulations in order?
Not exactly. Medicare enacts a penalty on hospitals that do not meet readmission goals. To meet the new goals, hospitals readmit patients, but they don’t label it “readmission“, they label it “observation“.
Elusive Search for Improvements
The Wall Street Journal explains how Medicare Rules Reshape Hospital Admissions.
At Banner Health’s general hospitals, the rate of heart-failure patients who wind up admitted to the hospital again soon after leaving has been dropping significantly, according to a Wall Street Journal analysis of Medicare billing data. So has the readmission rate for patients treated for pneumonia and three other serious conditions.
The Obama administration has cast such results as a triumph of the Affordable Care Act, which penalizes hospitals that have too many readmissions within 30 days of an inpatient stay. The goal is to encourage better follow-up treatment so patients can stay out of the hospital—keeping them in better health and whittling down the cost to the government.
But this seemingly good news isn’t as encouraging as it appears. At Banner, based in Phoenix, and at hospitals around the country, more patients are entering or re-entering hospitals under something called “observation status”—a category that keeps them out of the readmission tallies.
Patients on observation status can remain in the hospital for days, and typically receive care that is indistinguishable from inpatient stays, experts say. But under Medicare billing rules, the stays are considered outpatient visits, and as such, don’t trigger penalties under the health law.
The Journal’s analysis of Medicare billing data shows that increases in observation stays can skew the readmission numbers, letting hospitals avoid penalties even if patients continue to have complications and return for repeat visits.
Readmissions vs. Observations
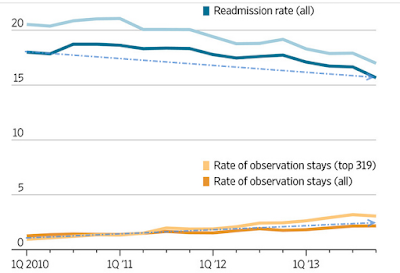
The above chart shows the top 319 hospitals compared to all the hospitals.
For the top 319 hospitals, as well a all hospitals in aggregate, as readmission rates fell, “observation” rates rose.
Who Pays for Obamacare “Observations”?
Medicare does not pay for observations. If patients don’t spend three days under formal inpatient admission in the hospital, the federal program won’t pay for a subsequent nursing-home stay. So patients pay out of pocket, and it can be very costly.
Shocking?
“We were shocked,” said Bob Wellentin, 87 years old, a retired teacher in Puyallup, Wash., who said he had never heard of observation stays before his wife spent four days in a hospital after a fall in June 2014. She recuperated for more than two months in a nursing home, costing the couple more than $20,000, according to billing records and receipts. To pay the bills, the couple liquidated a life-insurance policy and cashed in certificates of deposit set aside to pay for their burials.
Seniors Beware!
Please note that the Wellentin case does not even appear to be a readmission, but rather an initial stay after a fall!
That increases the need for awareness. Make sure you are being “admitted, not observed“. The difference can set you back $20,000 or more.
Shocking or not, I strongly suspect we still have not seen the end of these types of “improvement” revelations by the Obama administration.
Mike “Mish” Shedlock